Abstract
Introduction The European LeukemiaNet (ELN) reported 2022 guideline of the recommendation for diagnosis and management of acute myeloid leukemia (AML). Compared to 2017, ELN 2022 recommendation has some significant changes in risk classification. First, an exclusion of the FLT3-ITD allelic ratio in the risk classification, and FLT-ITD without NPM1 mutation is no longer classified as adverse risk because of the incorporation of FLT3 inhibitor. Next, in-frame mutations affecting the basic leucine zipper region (bZIP) of CEBPA regardless of monoallelic or biallelic is classified as favorable risk group. Another important change is the inclusion of myelodysplasia-related gene mutations, and patients with these gene mutations are now categorized as adverse risk group. The purpose of this study was to verify and compare the prognostic predictability between previous and new recommendation in the real world.
Patients and methods A total of 624 patients who were newly diagnosed with AML from October 1998 to October 2014 in seven institutions were included in this study. Patients who achieved complete remission (CR) received consolidation chemotherapy with or without allogeneic hematopoietic stem cell transplantation (HCT), depending on the availability of a matched donor. Genetic factors were not considered while considering allogeneic HCT.
Cryopreserved bone marrow or peripheral blood samples obtained at diagnosis were archived. Genomic DNA was extracted using QIAamp DNA blood mini-kits (Qiagen, Valencia, CA, USA) according to the manufacturer's protocol. Genetic profiling included the targeted deep sequencing of 45 genes, which had been selected based on recurrent driver mutations from previous studies. Agilent custom probes were designed to cover the entire exon regions of targeted genes and sequenced using an Illumina HiSeq 2000 sequencer. The threshold of mutation positivity was defined as a variant allele frequency≥2%.
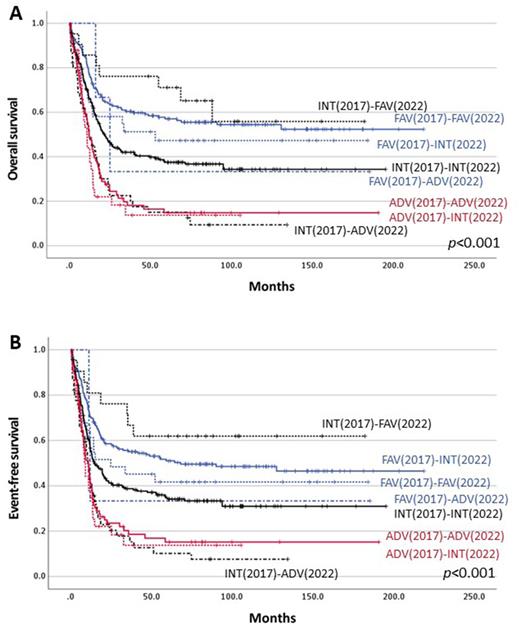
Results All of the 624 patients were older than 18 years and age with median age was 51 years (range 18-84). All patients were treated with induction chemotherapy using a standard 3+7 protocol, and 523 patients (83.8%) achieved CR. Among them, 235 patients (44.9%) proceeded to allogeneic HCT. After median follow-up of 84.4 months, median overall survival (OS) was 22.0 months and median event-free survival (EFS) was 16.2 months in all patients. By applying the 2022 ELN risk classification, each risk groups showed significant prognostic difference with Kaplan-Meier analysis of OS (P<0.001) and EFS (P<0.001) in all patients. According to ELN 2017 risk stratification, 218 patients (34.9%) were in favorable risk group, 298 patients (47.8%) were in intermediate risk group, and 108 patients (17.3%) were in adverse risk group. Among the previously favorable group, 31 patients were reclassified as intermediate risk group and 3 patients as adverse risk group, and there was no significant prognostic difference in OS (P=0.289) and EFS (P=0.279) between patients newly classified as favorable risk group and those reclassified as intermediate or adverse risk groups. But in patients without allogeneic HCT, favorable group by 2022 edition showed significantly longer OS (P=0.003) and EFS (P<0.000) than intermediate or adverse groups. Among the previously intermediate risk group patients, 21 patients were reclassified as favorable group and 46 patients as adverse risk group, and each group showed significant difference of OS (P<0.001) and EFS (P<0.001). Also, in adverse risk group patients by the 2017 edition, 33 patients were reclassified as intermediate risk group. Because the anti-FLT3 inhibitor therapy was not available at that times, patients who reclassified as intermediate group showed no survival difference compared to the patients remaining in the adverse group. The survival analyses comparing ELN 2017 and ELN 2022 are described in figure 1.
Conclusion ELN 2022 guideline is superior to the ELN 2017 for risk stratification and better predicts the prognosis of patients with AML in the real world.
Disclosures
Jang:AbbVie: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal